Tomorrow, Stroke experts will come together to share their expertise on this debilitating condition affecting millions. Stroke is the second most common cause of death after Ischaemia heart disease globally. In Sri Lanka due to our aging population the number of Stroke victims has risen sharply.
President of the Association of Sri Lanka Neurologists and Vice President of the National Stroke Association, Dr Harsha Gunasekera shares with the Sunday Observer his views on how to recognise, and minimize the risk of a brain attack by following some simple guidelines.
Excerpts…
Q. Stroke is one of the most devastating neurological diseases that leaves scarring impacts on victims for life. For our readers’ benefit, tell us what is stroke and what causes it?
 Dr Harsha Gunasekera |
A. Stroke is the commonest neurological emergency. Stroke occurs as a result of sudden disturbance of the blood supply to a particular area of the brain resulting in death or damage of the brain nerve cells. The mechanism is the same as with a heart attack, therefore Stroke can be correctly termed a “brain attack”.
Q. Are there different types of Stroke?
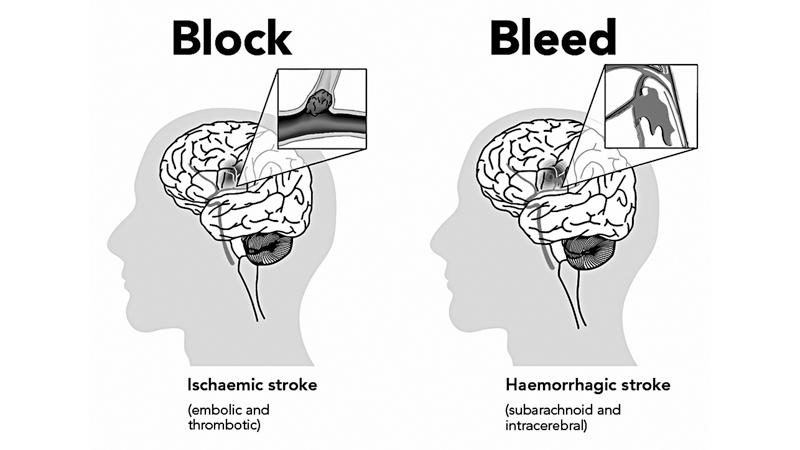
A. The disturbance of the blood supply in most patients (85%) occur as a result of blockage of a feeding artery (termed ischaemic stroke or infarction) and in others due to rupture of a feeding artery (termed haemorrhagic stroke).
Q. What is a Transient Stroke?
A Around a quarter of patients with Stroke may experience a Transient Ischaemic Attack (TIA or mini stroke). Here the symptoms of Stroke last only for a few minutes and then rapidly resolve. This condition should be given serious consideration and treatment initiated immediately as it may be the only warning one may get before developing a major Stroke.
Q. Does Stroke share the same risk factors as heart disease and other non communicable diseases?
A. Risk factors for Stroke and other non-communicable diseases such as heart disease and cancer are quite similar, smoking, unhealthy diet, obesity, heavy alcohol consumption, to name a few.
Q. What are the top NCDs that could trigger a Stroke?
A. They are heart disease, high blood pressure, diabetes, dyslipidaemia (abnormal blood lipid levels) and peripheral arterial disease affecting major feeding arteries of the brain.
Q. What are the early signs of the onset of a Stroke?
A. Knowing the “FAST” recognition of Stroke is the best way to remember the commonest signs of Stroke (see diagram). If any of the 3 signs are positive, the patient should be taken to the nearest major hospital immediately.
Q. What should be done when you get a Stroke?
A. Action must be taken immediately – rush to the nearest major hospital. Stroke Units are available in all teaching hospitals and most provincial general hospitals.
Q. What are the chances of recovery if treated early?
A. When you look at the Sri Lanka Stroke Clinical Registry data, only 16 % of patients arrived at the hospital within 3 hours which is the time limit to administer the clot buster injection. The reasons for this could be lack of awareness of Stroke signs or absence of pain in Stroke. Most patients with a heart attack rapidly seek treatment because of severe pain in the chest and receive lifesaving treatment. Even if there is no pain, Stroke should be considered as a “Brain Attack” and the patient brought to the closest major hospital.
Q. So if treated early, a patient recovers sooner with fewer complications?
A. Yes, this fact has been proven repeatedly in many research studies.
Q. What is the usual treatment procedure?
 A. The patient will undergo a quick clinical assessment to confirm the Stroke signs and then undergo a CT scan which helps to identify the type of Stroke (a brain bleed or blockage of a blood vessel). Clot busting treatment will be given to eligible patients after assessment. All patients are assessed for any abnormalities in blood pressure, oxygen and glucose levels and corrected if necessary. These factors affect Stroke of any type adversely.
A. The patient will undergo a quick clinical assessment to confirm the Stroke signs and then undergo a CT scan which helps to identify the type of Stroke (a brain bleed or blockage of a blood vessel). Clot busting treatment will be given to eligible patients after assessment. All patients are assessed for any abnormalities in blood pressure, oxygen and glucose levels and corrected if necessary. These factors affect Stroke of any type adversely.
All patients with Stroke will also be assessed and treated for possible complications such as infections (of the lungs and the urinary passage), DVT (clots in the leg veins), pressure ulcers and depression, which would adversely affect recovery.
Q. How long does a patient take to recover from a Stroke?
A. This is highly variable and depends on the severity of the Stroke and other co-existing disease states. Most patients with mild to moderate severity can be expected to recover within two weeks of onset. As a general rule after a Stroke one third of patients recover completely, another third will be left with a permanent disability and a third will die either in the acute stage or later from complications.
Q. What are the high risk groups for Stroke?
A. According to the World Stroke Organization data, 90 % of Stroke that occur are linked to 10 key risk factors. They are high blood pressure, smoking, diabetes, high blood cholesterol, irregular heart rhythm, lack of physical exercise, unhealthy diet, obesity, heavy alcohol consumption and lack of awareness about Stroke.
Q. Is it true that the age of the victims is now increasingly getting younger? Why?
A. Sri Lanka Stroke Clinical Registry data shows that 33% of patients were less than 60 years, still in their working life.
In a majority of these patients same risk factors that cause Stroke in the elderly play a role, which means people are acquiring conditions like high blood pressure, diabetes, high cholesterol levels and heart disease at a relatively younger age. Only a minority of young Stroke patients have other rare disease states that predispose them to Stroke.
Q. How do you prevent a Stroke?
A. As mentioned earlier according to the World Stroke Organization data, 90 % of Strokes are linked to 10 key risk factors. The important fact is that all of these risk factors are totally controllable. The initial screening for risk factors will need a consultation with a doctor and some basic tests. The next step is to carry out the advice on how to control your risk factors which will essentially include adaptation of a healthy lifestyle and if necessary some medications.
The easiest steps in maintaining a healthy lifestyle is to stay away from both active and passive smoking and take alcohol in moderation Next, maintain a normal body mass index (18.5 – 24.9) and healthy waist circumference (less than 40 inches for men and 35 inches for women). Do regular moderate physical exercise (e.g. walking) for 30 minutes a day for at least 5 days a week.
A healthy balanced diet – rich in fibre, fruits and vegetables and low in saturated fats, salt and sugar helps to maintain a healthy weight. Get your blood pressure, blood glucose and cholesterol levels checked and take treatment if advised by your doctor. Controlling your risk factors before developing a stroke reduces your lifetime Stroke risk by 80%.
Q. Once you get a Stroke is there always a danger of another Stroke?
A. Once you suffer a Stroke, your risk of a second Stroke increases significantly. Stroke Clinical Registry data shows 18% of patients had recurrent Stroke. So one needs to carefully continue all medications prescribed and maintain a healthy lifestyle to prevent another Stroke. If you adopt preventive measures, you can reduce your risk of getting another Stroke by 40%.
Q. I understand a new intravenous treatment called thrombolysis can reduce disability for Stroke if the patient is brought to a Stroke Unit within 3 hours. Is this available in Sri Lanka?
A. Yes, this (clot buster) treatment has been established in most major hospitals over the last few years. This is an expensive treatment, given free of charge at state hospitals. Unfortunately, in spite of awareness programs carried out by the Stroke Association, most patients miss the opportunity for treatment due to late presentation. In addition, clot retrieval treatment is being developed which can treat Strokes in selected patients even up to 6 – 12 hours from onset.
Q. How many Stroke Units are there in the country? Are they enough?
A. Most major hospitals now have either Stroke Units or dedicated beds in Neurology Units for the care of Stroke patients. Stroke Units do not require high tech equipment but mostly a defined area to care and rehabilitate the patients through a dedicated multi-disciplinary team which includes doctors, nurses, physiotherapists, speech and language therapists, occupational therapists, psychologists, social workers and nutritionists.
Q. What are the gaps you see in Stroke care that you would like to see filled?
A. Stroke is still the leading cause of adult disability and the 3rd leading cause of death in hospitalized patients. Prevention programs and more public education on Stroke need to be strengthened further.
Q. What has the Sri Lankan Stroke Association done to help Stroke victims so far?
A. It regularly carries out island wide public awareness and also conducts training programs for healthcare professionals on Stroke care throughout the country.
Q. Your message to the public in general and caregivers of Stroke patients.
A. Identify your own risk factors and follow the prevention guidelines detailed in this article. Care givers should ensure patients continue their medications and healthy lifestyle practices even after recovery, to prevent a future Stroke.

