Medically labelled DYSPHAGIA, is however not a rare condition. According to experts in Cerebral Palsy it is a common symptom which develops in children with moderate to severe Cerebral Palsy. Although dysphagia can happen to anyone at any age, children with Cerebral Palsy are more susceptible because the disorder affects the central nervous system.
 With the number of identified children with Cerebral Palsy (CP) in Sri Lanka now reaching beyond the 15,000 mark, health officials are concerned that care givers with no proper knowledge of how to feed such children and deal with them may do them more harm than good, unless they seek professional medical advice and supervision.
With the number of identified children with Cerebral Palsy (CP) in Sri Lanka now reaching beyond the 15,000 mark, health officials are concerned that care givers with no proper knowledge of how to feed such children and deal with them may do them more harm than good, unless they seek professional medical advice and supervision.
The Sunday Observer spoke to Chartered Physiotherapist and Founder Chairman of the Cerebral Palsy Lanka Foundation Dr Gopi Kitnasamy to enlighten us on this complex and little understood subject.
Excerpts…
Q. A child with Cerebral Palsy will likely face a number of health concerns during his or her lifetime. One of the most challenging of these concerns is what is medically labelled as Dysphagia. Not many people understand what this means. Could you explain what it is in laymen language?
A. Dysphagia is the medical term for difficulty in swallowing. Commonly referred to as oral-motor dysfunction, it is one of the most vexing challenges in terms of management for medical experts. Dysphagia is more common among children with moderate to severe cases of Cerebral Palsy. It is a dangerous condition that, if left mismanaged, can cause numerous life-threatening consequences, up to and including death – primarily due to the ability to block a person’s airway. For that reason, dysphagia must be vigilantly monitored by parents, caretakers and medical professionals.
Q. How is it linked to Cerebral Palsy?
A. Cerebral palsy is an umbrella term that refers to a group of disorders affecting a person’s ability to move. It is due to damage to the developing brain either during pregnancy or shortly after birth.
 Cerebral palsy affects people in different ways and can affect body movement, muscle control, muscle coordination, muscle tone, reflex, posture and balance.
Cerebral palsy affects people in different ways and can affect body movement, muscle control, muscle coordination, muscle tone, reflex, posture and balance.
Q. Who are most at risk ?
A. Although dysphagia can happen to anyone at any age , children with Cerebral Palsy are more susceptible because the disorder affects the central nervous system. When children develop this condition it is generally due to oesophogal problems. Symptoms vary from child to child.
Q. In what way?
A. Cerebral palsy can affect children differently. Some children may only have difficulties with posture, movement and coordination with little or no cognitive difficulties. Some children with cerebral palsy may experience difficulties with eating and drinking.
This may be due to the child’s inability to maintain his/her posture during mealtimes, difficulties with coordinating the muscles required for chewing food due to involuntary movements, spasticity, weakness or muscle spasms or limitations in the coordination needed for swallowing food or drink.
Q. How does that affect his/her eating and drinking abilities?
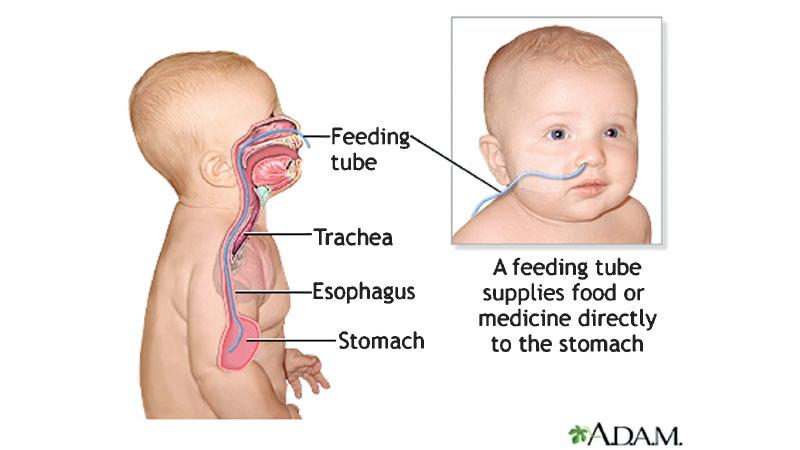
A. Because eating is a complex process involving neuromuscular competency. It involves the lips, jaw, tongue, palate and teeth as well as the voice box (larynx) or trachea, pharynx, epiglottis and oesophagus (gut). Children develop their eating and drinking skills with age. A child moves from breast-feeding or bottle-feeding to eating solid food and drinking from a cup independently.
While the process is developmental, each child’s age of acquisition of these skills is individual. Similarly swallowing is a complex neuromuscular process, whereby food from the mouth passes through the pharynx and esophagus into the stomach. It corresponds to swallowing food and saliva, and in general, in making it move from the mouth to the stomach, and applies to any liquid food (water, juice, milk), semi-solid (porridge, compote) and solids (biscuits, bread, meat).
Q. What sort of signs and symptoms should we look for to indicate the onset of Dysphagia?
A. Signs and symptoms vary based on the phase(s) affected and the child’s age and developmental level. They may include the following: Back arche/extensor pattern/increased spasticity/stiffness; breathing difficulties when feeding that might be signalled by increased respiratory rate; changes in normal heart rate (bradycardia or tachycardia); skin colour change such as, turning blue around the lips, nose and fingers/toes (cyanosis); temporary cessation of breathing (apnea); frequent stopping due to uncoordinated suck-swallow-breathe pattern; and desaturation (decreasing oxygen saturation levels). Also, coughing and/or choking during or after swallowing; crying during mealtimes; decreased responsiveness during feeding; difficulty chewing foods that are texturally appropriate for age; difficulty initiating swallowing; difficulty managing secretions; disengagement/refusal shown by facial grimacing, facial flushing, finger splaying, or head turning away from food source; frequent congestion, particularly, after meals; frequent respiratory illnesses; gagging; noisy or wet vocal quality during and after eating; taking longer to finish meals or snacks (longer than 30 minutes); refusing foods of certain textures or types; and vomiting (more than typical “spit-up” for infants).
Q. Any other issues that must be considered ?
A. Aspiration or respiratory issues – Among the most serious concerns a parent will have for a child with Cerebral Palsy, aspiration occurs when fluids enter the lungs, leading to infection. This can cause a person to choke, or close off an airway. Any of these situations can be life-threatening for a child, especially, one that is medically vulnerable.
 Q. How do doctors diagnose that a child has Dysphagia? What kind of tests are needed?
Q. How do doctors diagnose that a child has Dysphagia? What kind of tests are needed?
A. Clinical assessment involves a multi disciplinary approach. During clinical assessment, the multidisciplinary team observes the efficiency of the food boluscapture and preparation, the number of swallows, laryngeal elevation, the presence of coughing, choking or other suggestive signs of laryngeal penetration or laryngo-tracheal aspiration, oral escape of the food and nasal regurgitation, length of feeding, the presence of food residues in the oral cavity and changes in vocal quality after deglutition, as well as the need to use postural and/or facilitator manoeuvres.
Cervical auscultation is a method consisting of listening to the swallowing sounds to assess mainly the pharyngeal phase competence and its interaction with breathing through the use of a stethoscope.
A Video Fluoroscopic Swallow Study (VFSS) is a diagnostic procedure done under a moving X-ray (fluoroscopy) that furthers the clinical understanding of the swallowing process and swallowing mechanism.
Q. What is the treatment procedure, especially, since it involves young children?
A. A team approach is necessary for appropriately diagnosing and managing paediatric feeding and swallowing disorders. Postural and positioning techniques involve adjusting the child’s posture or position during feeding. These techniques serve to protect the airway and offer safer transit of food and liquid.
No single posture will provide improvement to all individuals, and, postural changes differ between infants and older children. Diet modifications consist of altering the viscosity, texture, temperature, portion size, or taste of a food or liquid to facilitate safety and ease of swallowing.
Adaptive equipment and utensils may be used with children who have feeding problems to foster independence with eating and increase swallow safety by controlling bolus size or achieving the optimal flow rate of liquids.
Tube feeding includes alternative avenues of intake such as nasogastric [NG] tube, transpyloric tube (placed in the duodenum or jejunum), or gastrostomy (G-tube placed in the stomach or GJ-tube placed in the jejunum). These approaches may be considered if the child’s swallowing safety and efficiency cannot reach a level of adequate function or does not adequately support nutrition and hydration.
Q. What do you see as the most serious outcomes if Dysphagia is not treated ?
A. Not treating dysphagia, or properly managing the condition, can lead to a number of health consequences like aspiration, respiratory issues/pneumonia, malnutrition and dehydration for a child.
Q. As Chairman and Founder of the Cerebral Palsy Lanka Foundation, have you found any positive outcomes and feedback you wish to share with our readers of the way children with Dysphagia have benefited in the past few years?
A. There is much research work happening in Dysphagia around the world and in neighbouring countries, which is a positive development. We will be starting some studies locally to learn more about the status of this condition and find solutions using the available resources in Sri Lanka.
Q. Your message to caregivers?
A. If the parents / caregivers see any indication that a swallowing issue exists, they must seek medical assistance immediately. When treated properly, dysphagia is a condition that can be managed, but it is something that must be evaluated, planned for and monitored properly.
