Cervical Cancer continues to remain a major public health concern among females despite most developed countries having reduced their incidence rate significantly in recent years due to good screening programs. In Sri Lanka too the National Cancer Registry has shown a minor drop in cervical cancer incidence rate following improvement of socio ecnomic status, new technologies and better cancer prevention and treatment . However, despite free cancer detection and treatment centres available the services are underutilized, laments Consultant Community Physician Dr Suraj Perera who discussed the available prevention and early detection services and how cervical cancer complications can be prevented, if detected early.
Excerpts of interview with the Sunday Observer …
 Q. What is cervical cancer ?
Q. What is cervical cancer ?
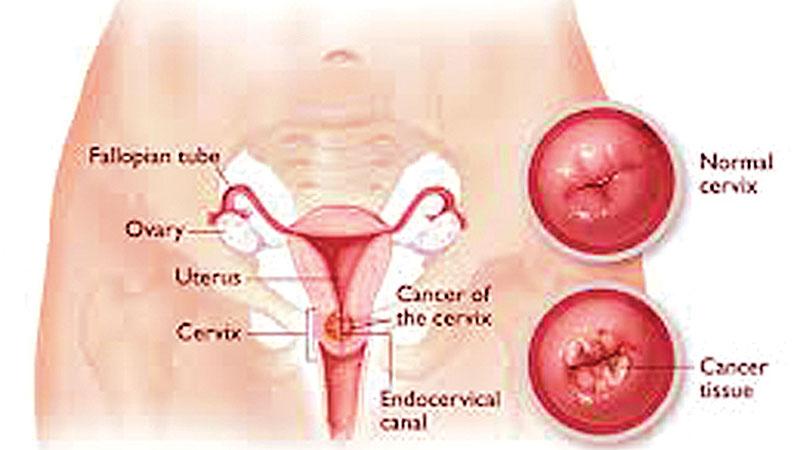
A. Cervix is the lowest part of the female womb (uterus) and the cancer originating from the cervix is called cervical cancer while the cancer originating from the body of the uterus is called Uterine cancer.
Q. What are the organs in the body that get affected due to cervical cancer?
A. Cervical cancer originates at the cervix and later it can be spread to other parts of the uterus or vagina. Also it can be locally spread to the rectum, bladder or urethra giving complications of bowel and urinary related complications at the advanced stage of cervical cancer, with devastating suffering.
Q. Cervical Cancer has been listed as one of the top five cancer sites in females after breast cancer, according to official statistics. Can you further describe that, using the latest statistics?
A. The statistics on newly detected cancer patients are obtained through the process called ‘cancer registration’. National Cancer Control Programme (NCCP) of the Ministry of Health coordinates cancer registration nationally.
The data on newly detected cancer patients are obtained from cancer treatment centres and pathology laboratories throughout the country. After receiving data from the above sources, the cancer registry staff process the data (including data coding, verification, data entering and analysis) to generate information on the cancer burden of the country.
Among the leading cancers in females, cervical cancer has continued to be in second position for more than two decades, being only surpassed by breast cancer. But in the interim report on cancer incidence data of year 2014 it was noted that cervical cancer was the third commonest incident cancer after breast and thyroid cancer as shown in table 1.
During 2014, 1,049 new cervical cancer patients were reported, which accounted for nearly 9 % among cancers reported in females during that year. Not detecting a single case of cervical cancer is a failure of the health system, since there are proven cost effective cervical cancer screening methods available to prevent the disease.
Q. Since the number recorded per 100,000 population is used to calculate the rate to compare cancer incidence over the time period, do you think there is an actual increase of cervical cancers?
A. According to the age standardized incidence rate of cervical cancer, cervical cancer incidence rate is not increasing over the time as shown in table 2.
Q. How about the global trend of cervical cancer?
A. About half a million new cervical cancer cases are detected per year globally and a quarter million females die due to cervical cancer. Nine out of ten cervical cancer deaths occurred in developing countries. In most of the developed world (especially the United Kingdom, Australia, Canada) cervical cancer incidence rate has reduced over the years due to good cervical cancer screening programs with call recall system.
Q. How does cervical cancer originate?
A. The cause of cervical cancer is persistent infection with one or more of the cancer causing (oncogenic) types of Human Papilloma Virus (HPV). About 70% to 80% of cervical cancers occur due to the persistent infection of HPV subtypes 16 and /or 18. There are other HPV subtypes which cause cervical cancer. HPV is transmitted to a female cervix through sexual contacts.
Therefore, when prevention of cervical cancer is considered, awareness on risk factors is important. The factors favouring HPV infection (having multiple sexual partners or having a partner with multiple sexual partners, commencing of sexual activity at an early age, having poor hygiene, having immunosuppressive status ) and factors favouring persistence of HPV infection ( tobacco smoking, poor socio economic status, poor nutrition status, high parity , prolonged usage of oral contraceptives, having immunosuppressive status ) need to be avoided.
Q. What are the signs and symptoms to look for in a suspected case of cervical cancer? How obvious are they at the initial stage? Is it true that there are no visible signs at the onset, unlike in breast cancer where you feel a lump?
A. Females having sexual contacts may get any sub type of HPV infection. Most HPV infections are transient. Only few HPV sub types are persistent at female cervix. Of them also a few sub types (e.g.HPV sub type 16 , 18) progress to precancerous lesions and invasive cancer.
There are no symptoms when a female is having an HPV infection or precancerous lesion. Cervical cancer has a pre cancerous stage which remains for 10- 20 years.
The symptoms and signs develop when a female develops an invasive cervical cancer. The early symptoms are: abnormal vaginal bleeding in between menstrual cycle , vaginal bleeding after sexual activity, vaginal bleeding after reaching menopause (post menopausal bleeding), unusual vaginal discharge….etc. If a female experiences these symptoms she should consult a doctor immediately for further assessment.
Q. How are they detected?
A. One of the main aims of cervical cancer prevention is promotion of females above 30 years having sexual contacts to undergo cervical cancer screening.
There are several screening tests available.
(i) Cytological test – Conventional Pap smear test or liquid based cytology test
(ii) Visual inspection of cervix using ascetic acid or Lugol’s iodine
(iii) HPV DNA test
The most available method in Sri Lanka is conventional pap smear test. It is available free of charge at Well Woman Clinics (WWC) throughout the country. More than 1,000 WWCs are established by the Ministry of Health. The details of the next WWC can be obtained from the closest Medical Officer of Health (MOH) Office or its staff {Medical Officer, Public Health Nursing Sister (PHNS), Public Health Nursing Officer (PHNO) , Public Health Inspector (PHI), Public Health Midwife (PHM)}. In addition to fixed WWCs established at field clinics, hospitals and MOH office, mobile WWCs can be arranged according to need at work places and other community settings after discussing with the local MOH.
In addition to WWC network free pap smear tests are offered at the selected gynaecology clinics or reproductive health clinics conducted at the main hospitals in the country.
Married females at the age of 35 are actively invited to attend the WWC for initial pap smear screening. After that if the report is normal females need to undergo pap smear tests at 5 year intervals, routinely.
For women who had undergone regular pap smear screening, further testing is not indicated after 65 years , if the last two screening results have been negative.
Pap smear test is a simple, quick and often painless procedure even though there is slight tolerable discomfort. Through this test cervical smear is obtained and checked by the cytologist under the supervision of Consultant Histopathologist.
Q. Are cervical cancer screening facilities available at the Cancer Early Detection Centre at Narahenpita?
A. Yes. Cancer Early Detection Centre is a walk-in clinic conducted on working days from 8.30 a.m.– 4.00 p.m. at the Narahenpita Junction (Colombo 5 ) by the National Cancer Control Program of the Ministry of Health.
It is a unique clinic where in house trained staff and facilities are available for early detection of cancers including pap smear test, HPV testing, Colposcopy facilities (for cervical cancer screening), Mammography testing (for breast cancer screening). Working populations are encouraged to attend this service for early detection of cancers.
Q. Are these tests available in the private sector?
A. Yes. Cervical cancer screening facilities are available at selected private hospitals. Also this test is included at the all cancer screening packages for married females.
Q. Many women who know about breast cancer and now take more precautions, still continue to remain ignorant about cervical cancer, and the services available free in state run hospitals. Why is this? Is it fear? Not wanting to know? Not knowing how to cope if the tests prove positive?
A. Even though cervical cancer screening facilities are available most of the females do not undergo cervical cancer screening.
Even public health staff especially the public health mid wife (PHM) actively campaigns to recruit all married females to undergo pap smear test at the age of 35 and 45, still the take up rate is not satisfactory as a country aiming at least 80% coverage of cervical cancer screening, of the target age groups .
Q. Is there still some kind of stigma regarding cancer in general that also contributes to this delay in women getting themselves examined for cervical cancer?
A. Our target is detecting pre cancerous stage of cervical cancers before developing to cervical cancer. By identifying at the precancerous stage, less invasive interventions can be taken.
Q. Is there an injection to prevent cervical cancer?
A. HPV vaccine is available for females before exposing to sexual contacts.
There are two types of vaccine registered in Sri Lanka.
Bivalent vaccine – HPV serotypes 16 and 18
Quadrivalent – HPV Serotypes 6, 11,16 and 18
According to clinical trial results, both vaccines are safe and very effective in preventing infection with HPV 16 and 18.
In Sri Lanka Quadrivalent HPV vaccine is given through the Expanded Program of Immunization (EPI) to female students at the age of 11. At schools two doses are given 6 months apart from year 2018 onwards
Immunisation against cervical cancer is not a substitute for regular PAP smears as immunisation does not cover all oncogenic HPV sub types.
Q. Your message to the public with focus on elimination of cervical cancer in particular?
A. The entire world has identified that cervical cancer can be prevented. Now even the United Nations, World Health Organization are advocating countries to develop strategies to eliminate cervical cancer as a public health problem.
While the governments are taking necessary measures, every citizen should support these initiatives. Individuals at recommended age need to undergo vaccination, cervical cancer screening while others need to encourage and facilitate those interventions.
