Twenty years ago, the National Stroke Association of Sri Lanka declared a National Stroke Day to create more awareness on this subject among the public. The rise in the number of new stroke admissions to hospitals and the fact that many of them are much younger than those in the past, has raised concern among neurologists who are now working together to prevent and give a better quality of life to patients already afflicted by stroke.
The Sunday Observer asked the President of the National Stroke Association of Sri Lanka, Dr. Harsha Gunasekara to explain what stroke is and how it can be prevented and treated.
Excerpts:
 Q. Today (Feb 28) is National Stroke Day. While Stroke is considered as one of the most debilitating conditions that could afflict any human being, not many or our readers still know what exactly a stroke is, or how and why it happens suddenly, often without any warning. Please define stroke in layman language.
Q. Today (Feb 28) is National Stroke Day. While Stroke is considered as one of the most debilitating conditions that could afflict any human being, not many or our readers still know what exactly a stroke is, or how and why it happens suddenly, often without any warning. Please define stroke in layman language.
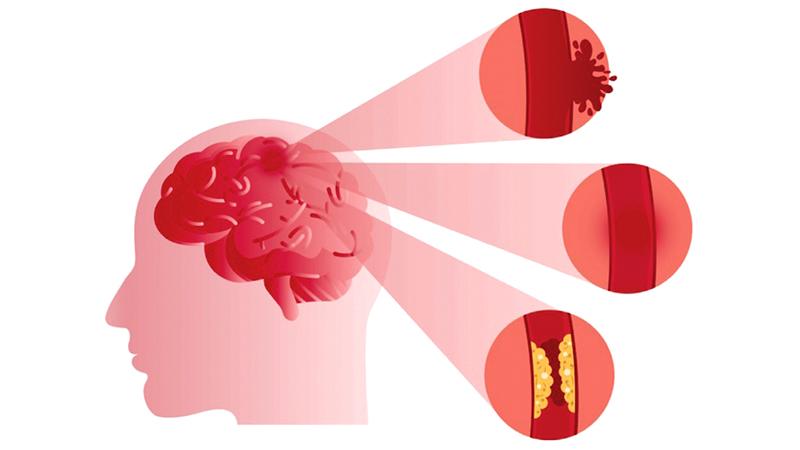
A. Stroke occurs due to a sudden disturbance of the blood supply to a particular area of the brain resulting in death or damage to the brain nerve cells. The mechanism is the same as with a heart attack. Thus stroke can be correctly termed a ‘brain attack’. It is estimated that 1.9 million nerve cells are destroyed every minute after a stroke and permanent damage could occur within a few hours.
Q. In the not too distant past, stroke was considered a disease of the elderly. Is this still true? Or do you see a new trend with younger patients now being admitted for stroke to hospitals in Sri Lanka? What is your latest update on this?
A. Preliminary data from the Sri Lanka Stroke clinical registry shows that 33 percent of patients were less than 60 years, still in their working life. In a majority of them the same risk factors that cause stroke in the elderly play a role, which means people are acquiring risk factors such as, high blood pressure, diabetes, high cholesterol levels and heart disease at a relatively younger age.
Q. What has caused this disturbing trend?
A. The major contributory factor for this is lifestyle changes with unhealthy dietary habits (consumption of fast and processed foods) and lack of exercise leading to a higher incidence of hypertension and diabetes at younger ages. Stress and unmanaged depression also play a role. Higher incidence of stroke is also seen in Asian populations.
Q. Why?
A. Modern busy lifestyles are usually associated with this trend.
Q. I understand that many factors lead to a stroke. What are the most important reasons that can cause a stroke?
A. Risk factors for stroke are non-communicable diseases (NCDs) such as high blood pressure, diabetes, abnormal blood lipid levels, irregular heart beat (atrial fibrillation) and disease affecting major feeding arteries of the brain. Lifestyle habits such as smoking, heavy alcohol use, unhealthy dietary habits, lack of physical exercise, stress and untreated depression increase the risk of stroke and other NCDs.
Q. Today a large number of people both young and old, in villages, towns and urban areas have switched to convenience foods such as takeaways and junk food which are high in fat, salt, oil and carbohydrates. Do you agree that this trend is one reason why more people are getting strokes at an earlier age?
A. Yes, this is the most common cause of stroke in the young. A minority of patients may have rare diseases predisposing them to stroke.
Q. Are those with low immune systems such as, diabetics, those with hypertension, cancer and heart problems more vulnerable to stroke?
A. Diabetes, hypertension and some types of heart diseases increase the risk of stroke. There is no direct link between stroke and low immunity and cancer.
Q. I understand there are different types of stroke. What are they?
A. The disturbance of the blood supply in most patients (85%) occurs due to blockage of a feeding artery (termed ischaemic stroke or infarction) and in others due to rupture of a feeding artery (termed haemorrhagic stroke). Around a quarter of patients with stroke may experience a Transient Ischaemic Attack (TIA or mini stroke). Here the symptoms of stroke last only a few minutes and then rapidly resolve. This condition should be given serious consideration and treatment initiated immediately as it may be the only warning one may get before developing a major stroke.
Q. Can stroke be mistaken for another disease with similar symptoms? What are the distinctive features that set it apart from other diseases with symptoms that resemble a stroke?
A. Yes, there are several ‘stroke mimics’ which need to be ruled out at the initial assessment. Important stroke mimics include low blood glucose levels, transient paralysis associated with certain types of seizures, migraine and hysterical paralysis.
Q. Are there early warning signs to look for before the onset of a stroke?
A. A most important feature is the sudden onset. A wide range of symptoms and signs may be seen depending on the area of the brain affected. Knowing the ‘FAST’ stroke scale is the best way to remember the commonest signs of stroke. If any one or more of the three signs are positive, the patient has very likely developed a stroke.
Q. Most of our readers are not familiar with the FAST stroke scale as a means of quick identification. Could you explain what it is and how it can be used?
A. This scale checks for three most common signs of stroke, they are:
F – Face: Look for facial drooping when the patient talks or smiles
A – Arms: Does the arm drop when asked to raise both arms
S – Speech: Is the speech slurred when talking
T – Time: If any one of these signs are present, take action immediately
Q. If we see these signs appearing in someone what is the first thing we should do? Who should we contact and where can we get the quickest response?
A. The patient should be taken to the nearest major hospital with a CT scanner, not the family doctor, even if the symptoms appear to be resolving. All Teaching, Provincial, District, General and most Base Hospitals have the facility. The 1990 Suwa Seriya Ambulance service is available to transfer the patient. Calling through 1990 mobile App will help quick identification of the location (available for free download).
Q. Where is the best place to get admitted for a patient with signs of stroke? Why?
A. The first step in the treatment is to identify the type of stroke by a CT scan. Therefore, the patient should be taken to a hospital with this facility. It doesn’t have to be a hospital with a stroke unit.
Q. I understand there are advanced techniques now being used for emergency management of a stroke such as, clot busting. Tell us about this technique? What does it involve?
A. This is done by administering an injection to dissolve the clot after careful evaluation of the patient.
Q. What category of patients are eligible for this treatment?
A. Patients with a blocked artery or ischaemic stroke, once all contra-indications are excluded.
Q. How long does this procedure take usually?
A. There are strict time windows for clot busting treatment for eligible patients which is 4.5 hours currently. However, patients need to reach the emergency units well in advance of this time period.
Q. What happens next?
A. Once the emergency management is done, the patients are admitted early to a stroke unit, a Neurology unit with dedicated stroke beds or a rehabilitation ward. A multidisciplinary team will manage the patient to minimise complications and disability and improve the patient’s functional capacity.
Q. Who comprises this team?
A. This team includes doctors, nurses, physiotherapists, speech and language therapists, occupational therapist and a social worker.
Q. Once a person gets a stroke will he/she be vulnerable to another stroke?
A. One in four stroke survivors are at risk of developing another stroke. All prescribed medications and lifestyle modifications should be meticulously continued.
Q. Prevention- how do you prevent a stroke? Any simple guidelines you can suggest?
A. Controlling the risk factors mentioned above will prevent 90 percent of all strokes. The first step is to see which of these apply to you and take measures to rectify them. The easiest would be to adopt healthy lifestyle habits which include diets rich in fresh fruits and vegetables, low in processed foods, and avoid high saturated fats, free carbohydrates and salt.
Q. Will exercise also help? If so for how long should one exercise?
A. Thirty minutes of physical exercise at least five times a week following your doctor’s instructions. Avoid smoking and keep alcohol use within safe limits. These will keep you away from stroke as well as other NCDs. Those who have NCDs should seek medical advice and control them.
Q. Many Lankans including children are now overweight. Is obesity a risk factor for early stroke?
A. Yes, a body mass index of over 24.9 and increased waist circumference (over 40 inches for men and 35 inches for women) increase the risk of stroke.
Q. We are now in the midst of a Covid-19 outbreak. Will a stroke victim be more vulnerable to this highly infectious disease than a normal person?
A. Pre-existing NCDs, especially, chronic lung and heart disease can increase the risk of infection. Preliminary data from countries with a heavy burden of Covid-19 has shown an increased risk of stroke and heart attacks due to increased risk of thrombosis.
Q. If a person with Covid-19 gets a stroke, what precautions do you have to protect the nursing staff, doctors and others attending to the patient?
A. Standard procedures of infection control and safety of all contacts apply here as well. Patients with NCDs need close monitoring to detect complications early and treat them.
Q. What are the Do’s and Donts in such a situation?
A. In this post-Covid-19 era, the most important advice is, continue all prescribed medications even if they are unable to attend clinics. We see a significant number of recurrent strokes due to non-adherence to preventive treatment. In the event of new stroke symptoms, getting to a hospital immediately is vital to obtain treatment on time.
Q. The Stroke Association of Sri Lanka is celebrating its 20th anniversary. Tell us some of the interventions your Association has put in place to help improve the quality of life of stroke victims in this country?
A. Our main objective is to reduce the burden of stroke in the country through improving public awareness of stroke, carrying the messages to the public that stroke is treatable if action is taken immediately and stroke can be easily prevented by adopting lifestyle changes. With the advances of treatment and availability of more stroke units, more patients now seek hospital treatment according to the data from annual health bulletins.
Q. What are your plans for this year and the near future?
A. Due to the Covid-19 situation, mass public awareness campaigns such as stroke walks will not be held. An awareness campaign through print, electronic and social media will be carried out instead. The Association is also liaising with the Health Ministry to establish more stroke units in provincial hospitals and a state-of-the-art National Stroke Hospital which will be set up in Colombo East.
Q. Your message to our readers on how to reduce their risks of stroke
A. The best advice I can give is to adopt healthy lifestyles and seek medical attention whenever necessary to prevent a stroke. Learn how to recognise a stroke easily so that you can help someone to seek treatment promptly and prevent adverse outcomes.
