Acouple of days ago, bone specialists across the world focused their attention on awareness raising and education among all sections of the community vulnerable to developing Osteoporosis (OP) which continues to remain a sidelined health issue in many countries including Sri Lanka.

Dr. Gunendrika Kasthuriratne
The Sunday Observer spoke to the College of Specialists in Rheumatology and Rehabilitation Sri Lanka, President and Consultant in Rheumatology and Rehabilitation, National Hospital of Sri Lanka Dr. Gunendrika Kasthuriratne to get an in depth insight into what OP means, how it develops and how it can be prevented with simple exercises, nutritious diets, and by making use of available resources Early Without Delay to avoid complications.
Excerpts.
Q: Just two days ago, we observed World Osteoporosis Day. What exactly is Osteoporosis?
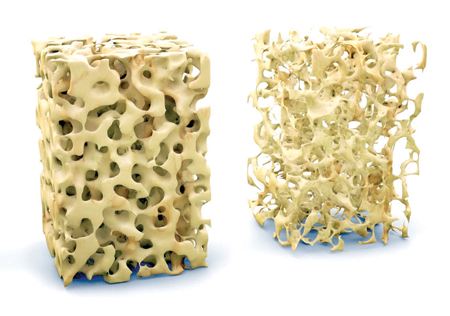
A. Osteoporosis is a condition where the density of your bones is less than normal. There is reduction of bone mass and deterioration of the architecture. The balance between bone formation and bone loss is lost. It can be primarily due to aging, or secondary to other diseases or some medications.
Q: The theme selected for this year is “Build Better Bones”. How are ‘better bones” linked to Osteoporosis (OP)?
A. Osteoporotic bones are not strong. The density is less, and the bone is fragile. The bone will break with minor falls. Hence the need to build better bones, which means stronger bones.
Q: Who are those most at risk of developing this condition age wise?
A. females are at higher risk of developing osteoporosis. When they reach menopause, they lose the hormone estrogen. Estrogen is necessary for the formation of bone. Therefore after the female stops menstruating (or when the periods stop), osteoporosis gradually sets in. In males the bone loss and osteoporosis starts around 70 years of age. Thin people are at higher risk than the obese. Lack of exercise too is a risk factor. Smoking and excessive use of alcohol are significant risk factors. Having dementia is also identified as a risk factor for OP
Q: Can OP occur in relatively younger persons?
A. Yes. There are several disease conditions which will predispose people for developing osteoporosis at any age. Examples are excess of thyroid hormone, excess of parathyroid hormone, diseases where the sex hormones (estrogen in females and testosterone in males ) are deficient, diabetes, inflammatory arthritis, chronic kidney disease and liver disease, malabsorption and persons who have organ transplants. Long term use of some medicines like prednisolone also accelerates OP.
Q: Since loss of bone is a leading contributor to OP, how early in life and at what age does this loss begin? From the mid 30’s upwards or earlier during adolescence?
A. Our body starts aging around 30 years. Bone loss also starts very slowly after 30 years.
Q: OP is also described as a disease which occurs silently and progressively. Do you agree? If so, what and where do the symptoms first appear?
 A. Osteoporosis is a silent disease, which means there is no pain in your bones due to osteoporosis. You will experience pain only if there is a fracture. Osteoporotic fractures occur with minor trauma. It is different from those which occur after falling from a height or at a road traffic accident. If you fall from your own height, you are at risk of getting a fracture. We have identified that those fractures from minor falls typically occur at the hip, spine, and wrist.
A. Osteoporosis is a silent disease, which means there is no pain in your bones due to osteoporosis. You will experience pain only if there is a fracture. Osteoporotic fractures occur with minor trauma. It is different from those which occur after falling from a height or at a road traffic accident. If you fall from your own height, you are at risk of getting a fracture. We have identified that those fractures from minor falls typically occur at the hip, spine, and wrist.
Q: Do they later spread to other parts of the body? If so, where?
A. Sometimes other sites like your pelvic bone and upper arm bone can fracture due to OP
Q: How do these injuries impact the patient? What are the negative consequences?
A. OP fractures can bring about grave outcomes. If the fracture is not treated properly and the victim is not brought back to walking, the bedridden ness will bring about many disadvantages.
Not only constipation, urinary tract infections and indigestion, but also frequent chest infections and blood clots in your calves which may be despatched from the leg up to the lung, bringing fatal outcomes. They might develop bed sores / pressure ulcers which are very difficult to treat. OP fractures occur in older adults who already have compromised organ systems. They can get strokes and heart attacks too due to lack of mobility.
Q: If allowed to progress without proper treatment can it lead to death?
A. Death is not directly due to the disease, but due to immobility related consequences after fractures.
Q: So how do we prevent it? What are the risk factors?
A. You can do little to prevent OP as it is part of aging. By having a good dietary calcium, vitamin D and regular exercise during adolescence you can achieve a higher bone reserve against future bone loss. In addition, you can prevent fractures by preventing falls.
Q: Can unhealthy lifestyles such as indulging in excessive alcohol consumption contribute to Osteoporosis?
A. It is evident from studies that excessive or chronic alcoholism is a clear predisposing factor for OP.. It is believed that heavy alcoholism can prevent calcium absorption and vitamin D absorption. Vitamin D nowadays is largely given as oral supplements. It may be affecting the function of bone forming cells and the function of the bone resorbing cells disturbing their balance. It is believed to reduce estrogen hormone in females, increasing the risk of OP. Estrogen is an essential hormone to stimulate bone tissue formation. And heavy alcoholism will predispose you to falls which will result in osteoporotic fractures.
Q: Smoking?
A. Smoking is a well-established risk factor for OP. It may reduce the levels of estrogen hormone in females. It may have a direct negative effect on bone architecture resulting in fragile bones.
Q: Can poor diets (that don’t contain much needed vitamins and calcium for growing bones as well as vitamin D and protein for older persons) cause OP?
A. Yes. A good diet rich in calcium and adequate vitamin D is very helpful to achieve a good bone reserve in early years of life. In older adults, a calcium poor diet and vitamin D deficiency will accelerate OP.
Q: Are the risk factors you just mentioned modifiable even if a person is already affected by OP? Can they be reduced or eliminated with proper rehabilitation and treatment?
A. Examples for modifiable risk factors for OP are vitamin D and calcium deficiency, smoking and excessive alcoholism, medical conditions like hyperthyroidism and hyperparathyroidism, which are treatable, body weight, regular exercise.
Q: What about non-modifiable factors such as. Genetics? If a person has a family history of OP what are the chances of him/her also developing this condition during his /her lifetime?
A. female gender, being a Caucasian are non-modifiable risk factors which can be considered as genetic factors. If a parent has had a osteoporotic hip fracture you have a non-modifiable risk of having an OP fracture with aging.
Q: Have you any simple guidelines that readers can follow regarding activities to be avoided to prevent OP risks?
A. Following are some of the many measures to take to prevent OP related fracture risks:
lIf patients have poor eyesight and hearing problems, they must be corrected.
* Arthritis can be treated to avoid falls.
* Inside the house, wet floors, rugs, carpets, wire cords across the floor, damaged floor tiles and unevenness of walking areas should be avoided. The corridors and washroom or toilet need good lighting during daytime as well as night. Grab bars can be fixed at the washroom and around the commode. Encourage older adults to use a bedside portable commode at night to avoid night time falls.
* Non-fitting slippers should be avoided.
* A walking aid should be used by people who have poor balance and neurological diseases.
Q: Activities to be encouraged?
A. Regular exercise and physiotherapy exercises if they have arthritis, soft tissue rheumatism, balance problems, muscle weakness or stiff joints.
A. Preventing falls is the most important.
When they grow old, they lose balance mechanisms, they are unable to prevent falling due to slow reflexes. Their eyesight is poor, and they will judge wrong about their own safety. They will have postural pressure drop as soon as they stand from lying or seated position, making them dizzy.
Q: What about medications that may cause dizziness leading to falls?
A. We must be cautious when prescribing medications which are known to cause sedation or dizziness in older persons. If we have no other choice, it is very important to warn the patient and the carer about those side effects. It is advised to avoid polypharmacy in the elderly because not only the drug side effects, but also the interactions between those multiple drugs can cause dizziness.
Q: Explaining to a vulnerable person how OP is caused, its risk factors, and its negative outcomes is being advocated by the present global campaign to raise awareness early. What is your take on this?
A. A must do. The family members or carers too should be targeted here.
Q: If already at risk, what do you suggest as the first thing a suspected patient should do?
A. They should get medical advice to test for osteoporosis. An Xray of the spine is necessary to check whether they are already having a fracture. OP fractures in spine can occur without falling, and can also be painless or can cause mild pain only. A Dexa Scan is necessary to screen them otherwise.
Q: OP, like other diseases, requires teamwork. Who comprises the team that specialises in dealing with the rehabilitation of OP patients?
A. OP needs rehabilitation only if they get fractures. Rehabilitation teams consist of at least, a doctor, physiotherapist, and an occupational therapist.
Q: Gaps in the present health system regarding optimal care for OP patients which you wish to see filled?
A. Many patients are not brought to a hospital after fractures, resulting in several cases with malunion or nonunion of fractures.
Those late presentations are difficult to rehabilitate. And in some instances, rehabilitation is not connected after fracture treatment. Patients are still in wheelchairs after surgical treatment resulting in pain, stiff joints and immobility .
They need to understand that with rehabilitation with physiotherapy and occupational therapy, they can come back to normal functioning.
Q: Have you a message for our readers on preventing or minimising risks of OA?
A. Do not have to be frightened of OP. It gives no pain without fractures. Fractures will not occur (except those in the spine) suddenly or spontaneously without falling.
Encourage a healthy diet and adequate exercise for young adults. They need to build a good reserve of bone against future bone loss with aging.
Be aware of the OP risk in all females after menopause.
Vitamin D is deficient in the majority of people.
Take vitamin D supplements and calcium (in food or with supplements), before and after menopause. Keep fit with exercise and balance training when you age.
Be aware of falls prevention of the older adults.
Females should get screened for OP during the first 10 years after menopause.









