Cleft lip and or palate (CL/P) is one of the commonest birth defects involving the regions of head and face, which may occur one in every 700 babies.
The emotional impact on parents at the birth of their new-born with CL/P can be traumatic especially to the mothers, and may affect the sensitive early parent-child relationship. Therefore, it is important for women in reproductive age, to be aware of this condition as it can help prevent complications in breastfeeding and improve the child’s quality of life.
What is Cleft Lip and Palate?
During early pregnancy, different areas of the face of the embryo develop separately and later join together. Failure to join properly results in a “cleft” which means a split or separation, in the lip, palate or both.
The exact cause/reason for this defect is not known. It can be classified as,
1. Syndromic clefts (cleft associated with a syndrome, eg: Van der Woude syndrome)
2. Non – syndromic clefts ( sporadic clefts) – Multifactorial and complex
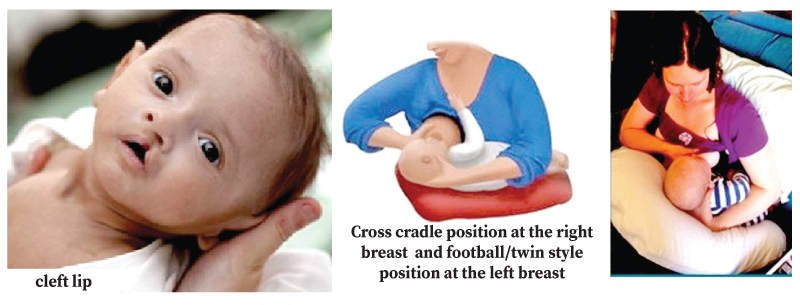
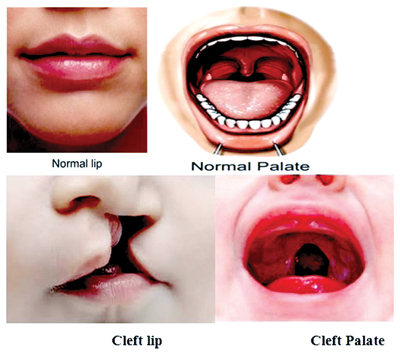
Types of cleft lip (CL)
It is a split in the upper lip below the nose. It may range from a slight dimple or notch in the upper lip to a complete separation up to the nose either on one side or on both sides.
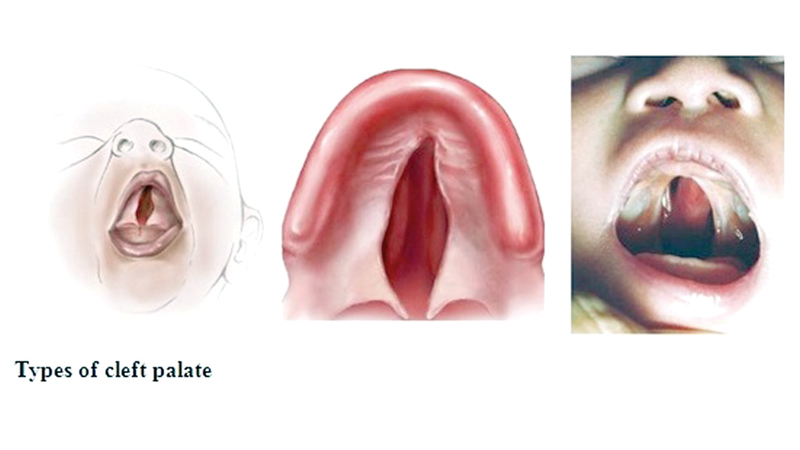
Types of cleft palate
It is a split in the palate or roof of the mouth. It may range from a slight separation of the soft palate to complete separation, either on one side or on both sides up to the hard palate.
Normal physiology in breastfeeding
 Babies use suction to breastfeed successfully. The ability to generate suction is necessary for attachment to the breast, and to maintain a stable feeding position. During sucking, the lips flange against areolar, sealing the oral cavity anteriorly. The soft palate rises up to contact the pharyngeal walls and seal the oral cavity posteriorly. Then the tongue and jaw drop, so that the oral cavity increases in size.
Babies use suction to breastfeed successfully. The ability to generate suction is necessary for attachment to the breast, and to maintain a stable feeding position. During sucking, the lips flange against areolar, sealing the oral cavity anteriorly. The soft palate rises up to contact the pharyngeal walls and seal the oral cavity posteriorly. Then the tongue and jaw drop, so that the oral cavity increases in size.
It will lead to generate negative oral pressure, drawing milk from the breast. Suction and wave-like movement of the tongue help to transfer and deliver milk during breastfeeding.
Why breastfeeding can be difficult for a baby with CL/P?
Infants with CL/P have difficulty in sucking and generating negative pressure in the oral cavity. The lips do not seal around the nipple adequately when there is a cleft in the lip.The oral cavity cannot be adequately separated from the nasal cavity when there is a cleft palate. Some rare conditions associated with clefts also can make the baby tired and sucking less effective (Heart problems, respiratory problems and muscle weakness.)
It is a known fact that mothers having children with no congenital/anatomical abnormalities also face breast feeding difficulties. Having a CL/P brings multiple challenges to the mother as well as to the baby from birth. Breastfeeding can impose significant stress, an emotional and physical burden to the mother that might lead to lack of confidence in initiating and continuing feeding the baby. The maternal anxiety and frustration may negatively affect the bond and interaction between the mother and the infant.
Difficulties the baby might face
Infants who have cleft palate have a higher risk of having breastfeeding difficulties than infants with cleft lip only, since they lack the ability to generate adequate negative pressure in the oral cavity and a suckling effect on the area around the nipple ( areolar)
Complications can take place during breastfeeding such as,
* Fatigue during breastfeeding.
* Prolonged feeding times
* Milk coming through nose
* Milk vomiting
* Not getting adequate milk from the breast.
* Choking during feeding
* Swallowing of air leading to colic.
* Severe dehydration
* Middle ear infections ( Otitis media)
* Aspiration related lung complications
* Impaired growth and failure to thrive
The success of a breast feed depends on,
1. Size and the type of the cleft
Infants with Isolated cleft lip or small soft palate clefts often successfully breastfeed because they can generate suction and negative oral pressure. But others with larger soft/hard palate clefts cannot generate adequate negative pressure, leading to less success rates in breastfeeding.
2. Maturity of the infant
Term and preterm newborns may generate lower suction than older infants.
3. Educational level of the mother
Less educated mothers depict low confidence levels in breastfeeding. And lactation counselling for such mothers will increase their confidence.
How to breastfeed babies born with clefts
* Babies’ with CL/P should be first evaluated by trained medical staff, on an individual basis, taking into consideration the size and the location of the cleft and as well as mother’s wishes, previous experience with breastfeeding and support.
* If there is no risk of milk aspiration, breast feeding should be initiated as soon as possible after the birth under supervision of a trained personnel. Baby is put to the breast initially and observed if the baby is capable of sucking at the breast.
* Breastfeeding can be continued if there are no signs of aspiration, desaturation and cyanosis. If episodes of desaturation are detected, the baby should be admitted to the PBU and fed via a nasogastric tube, since it has no risk of aspiration.
* Hydration and weight gain is monitored while the feeding method is established.
Helpful breastfeeing positions
The following positions have been found to be helpful to breastfeed CL/P babies.
* For babies with only a cleft lip at right side – Cross cradle position at the right breast and football/twin style position at the left breast
* For babies with a bilateral cleft lip ( both sides of the lip) -“Straddle position” / face on
* For babies with cleft palate or combination of clefts in lip and palate – Baby should be breast fed in a semi- upright position. It will reduce nasal regurgitation and flow of milk to eustachian tubes. Twin/football position is more effective than cross cradle position.
Advice
* Breastfeeding is always promoted and bottle feeding is discouraged. In such instances where breastfeeding is not possible due to the defect, expressed breast milk can be given to the infant via a special orthodontic bottle with a special teat (obturator teat). This decision should be always taken by medical personnel after assessing the infant thoroughly.
* Feeding with a cup is never recommended since it has a high risk of aspiration through the palatal defect.
* First surgery for cleft lip closure is usually done in around 3 months. If the surgeon recommends, breast feeding can be continued without imparting stress on the surgical site.
* If there is weight loss and inadequate milk transfer, complementary feeding can be started at around four and half months, without starting formula feeds.
* Lactation counselling plays a major role in educating the mother regarding correct breastfeeding positions and attachments. The mother is made aware that sucking stimulates breast milk production while assuring a continuous milk flow. Her psychological stress, anxiety and fear would also be addressed during breastfeeding counselling.
It’s true that CLP is a challenge to the baby, parents and the family. The mother of the baby will have a long road ahead. The baby will need feeding support in addition to ongoing care with regular hearing checks, speech therapy, dental and orthodontic work and sometimes plastic surgery. Undoubtedly, this will be a successful breastfeeding journey, for a mother dedicated to the purpose.