 Despite the ongoing battle to eliminate HIV/AIDs, it remains a global public health issue. The Sunday Observer spoke to Consultant HIV and Sexual Health Physician, Matale STD/AIDs Unit STD/AIDS Control Programme, Dr. Iruka Rajapaksha to find out the new challenges faced by the HIV/AIDs community and how they could be met to ensure a better quality of care for all patients across the country including those in remote towns and rural cities.
Despite the ongoing battle to eliminate HIV/AIDs, it remains a global public health issue. The Sunday Observer spoke to Consultant HIV and Sexual Health Physician, Matale STD/AIDs Unit STD/AIDS Control Programme, Dr. Iruka Rajapaksha to find out the new challenges faced by the HIV/AIDs community and how they could be met to ensure a better quality of care for all patients across the country including those in remote towns and rural cities.
Excerpts
Q: December 1 is World Aids Day. Why is a special day dedicated to this particular health issue amidst so many other pressing health problems?

Dr. Iruka Rajapaksha
A. It is because HIV still remains a major global public health issue, having claimed nearly 40 million lives so far with ongoing transmission in all countries globally.
Q: As many people still don’t know the basic facts about how HIV is caused and transmitted, could you explain to them what HIV is and how it is spread?
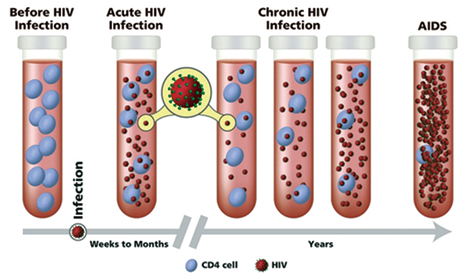
A. HIV (Human Immunodeficiency Virus) is a virus that attacks the body’s defensive system. Over the years the immune system gets weaker and progresses into AIDS (Acquired Immune Deficiency Syndrome) stage. HIV can be transmitted via the exchange of a variety of body fluids from people living with HIV, such as blood, breast milk, semen and vaginal secretions therefore predominantly through sexual contact. HIV can also be transmitted during pregnancy and delivery to the child.
Q: The theme for this year is “Let Communities Lead”. Why was it chosen and how does it help the HIV/AIDs community?
A. Ending AIDS needs collective response from government and non-governmental organisations as well as civil society participation. December 1 offers an opportunity for communities to encourage progress in HIV/AIDS prevention, treatment and care around the world.
Q: How many patients does Sri Lanka have at present living with HIV or with AIDS?
A. Adult HIV prevalence in Sri Lanka is less than 0.1 percent. At the mid 2023 cumulative 5,357 cases were reported in Sri Lanka.
Q: Has there been an increase since then?
A. An estimated number of people living with HIV in Sri Lanka are increasing gradually due to various factors such as increased testing, more case detection and better reporting. As HIV replication can be effectively controlled with antiretroviral therapy, those who begin treatment have longer, higher-quality lives with near normal life span. Hence the overall number of persons living with HIV in the nation is rising.
Q: Who is most at risk of getting infected gender- wise and age-wise?
A. According to the numbers reported in 2022 male to female ratio is 7:1. While female numbers have remained static during the past five years, infections among males are increasing.. The trend in reported HIV cases also represents a younger age group and most of them were young men.
Q: Why?
 A. Young people are not aware of the risk of HIV. Lack of information about sexual health services further puts them at risk. A liberal attitude to sex makes young people seek sexual pleasure in different ways. Unprotected anal sex carries the highest risk for HIV infection. Oral and anal sex can cause other sexually transmitted infections such as genital herpes, genital warts, gonorrhoea or syphilis. We need more action to be taken to reach young men to promote safer sex.
A. Young people are not aware of the risk of HIV. Lack of information about sexual health services further puts them at risk. A liberal attitude to sex makes young people seek sexual pleasure in different ways. Unprotected anal sex carries the highest risk for HIV infection. Oral and anal sex can cause other sexually transmitted infections such as genital herpes, genital warts, gonorrhoea or syphilis. We need more action to be taken to reach young men to promote safer sex.
Q: Occupation wise who are most at risk?
A. Sex workers, men who have sex with men, people who inject drugs, transgender people and prisoners are considered as key populations for HIV spread worldwide. Similarly, the few groups identified locally as most at risk of HIV infection are men having sex with men, female sex workers, transgender people, people who inject drugs, beach boys and people in closed settings (Prison inmates). They are at risk as they have unprotected sex with many partners. They have a risk of getting infected and are capable of infecting others. Men who have sex with men account for the majority of new HIV diagnoses. They are at higher risk for acquiring HIV because anal sex is the riskiest type of sexual intercourse for contracting or transmitting HIV.
Q: What are the symptoms of early onset of HIV?
A. Most people infected with HIV experience a short, flu-like illness that occurs 2-6 weeks after infection. However, early HIV infection does not cause significant symptoms to give a clue to the diagnosis. After this, HIV may not cause any symptoms for several years. When a person gets infected with HIV the person may remain free of symptoms for the next 8-10 years. Therefore, people should not wait for symptoms to appear if they perceive a risk for acquisition of infection.
Q: If detected early and treated in time can HIV be cured? Or reversed? How?
A. If someone has had risky unprotected sexual exposure, it is important to get a blood test for HIV done. HIV infection can be well controlled following early diagnosis. However, HIV cannot be eliminated from the body. Treatment can only control viral multiplication and transmission. If the viral level is low the infected person’s immunity is high. A person who is taking treatment satisfactorily will not develop AIDS.
When HIV drugs are prescribed, they can reduce the amount of HIV viral load in a person’s blood to a level that is too low to measure. This is called undetectable. Remaining undetectable prevents HIV from progressing and allows people to live long and healthy lives. It also protects the health of their sexual partners. People cannot transmit HIV through sex if they have an undetectable level of HIV. This is estimated to be 100 percent effective as long as a person with HIV takes the medication as directed and remains undetected. This concept is known as Undetectable = Untransmittable (U=U).
Q: How is he diagnosed? What are the tests used?
 A. There are few types of screening tests. One of them is used as the initial test. If it becomes positive further testing is arranged. When the confirmatory tests are positive the patient is informed of the HIV positive status through post-test counselling.
A. There are few types of screening tests. One of them is used as the initial test. If it becomes positive further testing is arranged. When the confirmatory tests are positive the patient is informed of the HIV positive status through post-test counselling.
Q: Does it need a hospital setting for these tests ? Or can it be done in a mobile clinic?
A. HIV testing facilities are available free of charge in STD clinics in all major hospitals. Testing facilities available in private hospitals and laboratories as well. The National STD AIDS Control Program collaborates with non-governmental organisations for community testing via mobile clinics. If the screening test becomes positive, the patient will be referred to a local STD clinic or the clinic he wished to attend.
Q: If tested positive what is the treatment procedure?
A. If the HIV status is confirmed, patients will be counselled further regarding the services available and the support provided for people living with HIV. Doctors and other staff at the STD clinics are aware of the psychological impact of the diagnosis and try their best to support patients during this period. Antiretroviral treatment is started as soon as possible.
Q: What happens if a person with suspected symptoms fails to get tested in time?
A. Without early detection and treatment, HIV progresses to the most serious stage of AIDS. Then your immune system is so weak that you cannot fight infections.
Q: Are there different stages in the progression of the disease?
A. There are three stages of HIV infection are (1) acute HIV infection, (2) chronic HIV infection, and (3) acquired immunodeficiency syndrome (AIDS).
Q: Are there different stages in the progress of the disease?
A. AIDS is the final, most severe stage of HIV infection. Once a person is diagnosed with AIDS, they can have a high viral load and are able to transmit HIV to others very easily. Without treatment, people with AIDS typically survive about 3 years. At the final stage HIV has severely damaged the immune system, the body cannot fight opportunistic infections and infection-related cancers that occur more frequently or are more severe in people with weakened immune systems. Recurrent severe respiratory tract infections, Tuberculosis, fever that lasts more than 10 days, weight loss with no obvious reason, severe, long-lasting diarrhea, yeast infections in mouth, throat are some examples.
Q: Is there a global target for ending HIV? I understand that UNAIDS has identified the global target for ending AIDS in 2030. How does the Ministry of Health plan to achieve this target? Outline some of the latest interventions to this effect.
A. The National Strategic Plan 2023-2027 is developed to advocate for continued commitment by all stakeholders to achieve the country’s pledge to reach the 2030 target of ending AIDS as a public health threat. The plan outlines a set of national priorities giving special attention to prevention of new HIV infections especially among key populations. Identified key interventions include scaling up of HIV testing services, prevention technologies such as pre-exposure prophylaxis, condom promotion, HIV treatment as prevention, supportive environment which protects and promotes human rights and gender equality and strengthening health and community.
Q: Gaps in the present health system regarding the delivery of optimal care for HIV /AIDs patients which you now see ?
A. The main point is the concern that HIV is not seen as a problem in Sri Lanka. Since we have a low prevalence of HIV people get a false sense of security. They feel they are not at risk and their partners are free of infection. Due to this low perception of risk people are not concerned about prevention strategies and get infected with HIV. At the same time, health care worker initiated or voluntary uptake of HIV testing is also not up to the expected level. We need to bridge these gaps in testing.
Q: How would you like to fill them?
A. We need to work to increase access to essential HIV services for key populations and the general public. In addition, scaling up of coverage and quality of sustainable sexual health services.
Q: Myths about HIV/AIDs?
A. People living with HIV can live a normal life if they take treatment regularly. They can continue their employment, can look after their families and get engaged in social activities. There is no reason to treat them differently. HIV is not transmitted through close social contacts like hugging, shaking hands, sharing toilets, sharing dishes or kissing with someone who has HIV. People living with HIV need others’ support to live a normal life without stigma and discrimination.
Q: Your message especially to young people leading risky lives ?
A. Youth is the hope for the future. Enjoy your youth with proper understanding and knowledge. Once you are infected with HIV, it cannot be reversed. Yes, the virus can be controlled with existing treatment. But there are many things you can do to prevent getting HIV infection. Perceive your risk of HIV and be aware that if you get it you have to live with it for a life time.
Many youth-friendly sexual health services are available through STD clinics throughout the island. Know4sure.lk is an online reservation system that aims to provide the most convenient means to make reservations for sexual health services including HIV testing with the preferred STD clinic while handling your data to ensure anonymity and privacy.






