 Monkeypox (MPOX) is reportedly spreading in many parts of the world including South Asia with cases being detected in Pakistan prompting India to send a red alert to the public to take precautions against being infected by this emerging disease.
Monkeypox (MPOX) is reportedly spreading in many parts of the world including South Asia with cases being detected in Pakistan prompting India to send a red alert to the public to take precautions against being infected by this emerging disease.
The Sunday Observer spoke to Consultant Medical Virologist and Senior lecturer, Faculty of Medicine, University of Colombo, Dr. Ishara Premathilake for more insights to this emerging disease.
Excerpts.

Dr. Ishara Premathilake
Q: While no cases have yet been confirmed in Sri Lanka , Lankan healthcare workers and officials have expressed concerns/worries that it could soon find its way here due to travel bans being lifted and the likelihood of people from infected countries visiting the country while knowingly or unknowingly carrying the virus in them and thus infecting non infected persons who come into close contact with them. Do you agree?
A. With the increased rates of foreign travel, this is technically true for any infectious disease. That is why we need to raise awareness among both the healthcare workers and the general public and be prepared to manage it successfully
Q: As a virologist explain briefly to our readers what mpox is as it is a new disease and most people still don’t understand.
A. In short, mpox is an infectious disease caused by the monkeypox virus. The disease was previously known as monkeypox disease but now the terminology has changed..
If we talk about the monkeypox virus (MPXV), it belongs to the same virus family,’Poxviridae’ as the smallpox virus, but causes a milder disease.
Q: Where was it first discovered?
A. The first human case was reported from the Democratic Republic of Congo (DRC) in 1970. The disease is endemic to central and west Africa.
Q: Who are the most common carriers?
 A. It spreads from person to person or occasionally from animals to people. The natural reservoir of the virus is unknown – various small mammals such as squirrels and monkeys are susceptible.
A. It spreads from person to person or occasionally from animals to people. The natural reservoir of the virus is unknown – various small mammals such as squirrels and monkeys are susceptible.
Q: What are the different genetic types of the virus and why are they important?
A. There are two main genetic types (genetic clades) of the virus known as clade I and II. Clade I causes more severe illness and deaths. Some outbreaks have killed up to 10 percent of infected patients, although more recent outbreaks have had lower death rates. Clade I is endemic to Central Africa.
Clade II caused the multi-country outbreak in 2022. Infections from clade II are less severe and less infectious. More than 99.9 percent of people survive. Clade II is endemic to the West.
Africa. In the 2022 outbreak most cases were spread through sexual contact, particularly among men who have sex with men.
Now a new virus strain has emerged causing concerns globally
Q: Tell us more about the new variant? How dangerous is it compared to the previous one?
A. The new variant of clade I MPXV, known as clade 1b, began in Central Africa in late 2023. As of August 2024, more than 17,000 cases have been reported, with over 500 fatalities (~3 percent fatality rate), nearly all in the DRC. Cases were reported from countries where mpox was not endemic including, Burundi, Kenya, Rwanda, and Uganda, Ivory Coast and Sweden. Due to the potential risk of rapid growth of cases due to this new strain of virus, the WHO declared a PHEIC in August 2024. Comprehensive data on the behaviour of the new strain is still lacking. Recently, a few cases of mpox were reported in Pakistan, but none of these were due to clade Ib virus according to the available information.
Q: What do the symptoms look like?
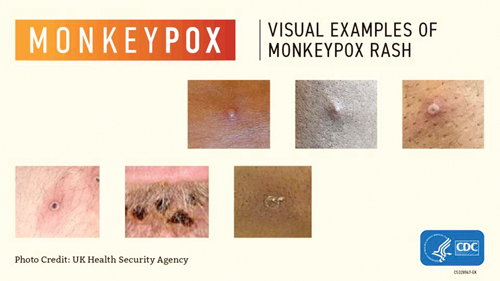
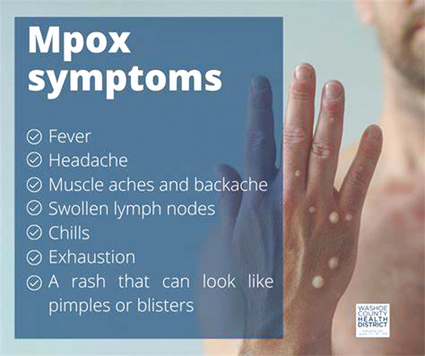
 A. Mpox can cause a range of signs and symptoms. While some people have less severe symptoms, others may develop more serious illness and death. Common symptoms include a blistering (vesicular) rash lasting for 2–4 weeks. This is usually preceded by a prodromal period characterised by fever, headache and general unwellness.
A. Mpox can cause a range of signs and symptoms. While some people have less severe symptoms, others may develop more serious illness and death. Common symptoms include a blistering (vesicular) rash lasting for 2–4 weeks. This is usually preceded by a prodromal period characterised by fever, headache and general unwellness.
Patients may also notice enlarged lymph nodes. The rash progresses through macular, papular, vesicular, and pustular stages before scabbing over and desquamation. The rash appears first and is more dense on the extremities of the body such as face, palms of the hands and soles of the feet. Groin, genital and/or anal regions also can get affected. Mucosal surfaces such as the mouth, throat, anus, rectum, genitalia and eyes may get affected. The classical mpox due to clade I is notorious to give rise to a more severe rash with hundreds or thousands of lesions all over the body, while clade II infections usually cause a less severe disease, commonly localised to genital areas, rectum and mouth.
Q: Can anyone contract it?
A. Yes, if they had an adequate exposure. Newborn babies, children, pregnant women and immunodeficient patients may be at higher risk of severe disease. Symptoms in children are similar to adults.
Q: What are the main complications of the disease?
A. Complications include severe bacterial infection of skin lesions and severe pain of genitalia and anal/rectal area with rectal bleeding. Scarring of the affected areas particularly genitalia, urethra, rectum and eyes can cause functional impairment.
Q: Can a person who has been exposed to an infected person during the incubation period get the disease?
A. The incubation period is the time between exposure to the infection and the development of symptoms. This is usually 5-21 days for mpox (average 9 days.) A person is unlikely to be contagious during this period. However, patients may be infectious during the prodromal period, when they experience fever and general unwellness.
Q: How does the disease spread from person to person?
A. The virus can spread through close contact. This includes skin-to-skin (such as touching or sex) and mouth-to-mouth, or mouth-to-skin contact (such as kissing).
It can also spread from face-to-face contact (such as talking or breathing close to one another, which can generate infectious respiratory particles) for a prolonged period. This may happen while sitting next to an infected person during air travel.
 During the 2022-2023 global outbreak, the virus predominantly spread through sexual contact. More research is needed on how mpox spreads during the current outbreak, People with mpox are considered infectious until all their lesions have crusted over, the scabs have fallen off and a new layer of skin has formed underneath, and all the lesions on the eyes and in the body (in the mouth, throat, eyes, vagina and anus) have healed too.
During the 2022-2023 global outbreak, the virus predominantly spread through sexual contact. More research is needed on how mpox spreads during the current outbreak, People with mpox are considered infectious until all their lesions have crusted over, the scabs have fallen off and a new layer of skin has formed underneath, and all the lesions on the eyes and in the body (in the mouth, throat, eyes, vagina and anus) have healed too.
Q: Do bed sheets, blankets and other items used by an infected person raise risks of developing the infection in a non-infected person?
A. There is a possibility, particularly if the exposed persons have any cuts or abrasions or touch their eyes, nose, mouth or other mucous membranes without first washing their hands.
Cleaning and disinfecting surfaces/objects and cleaning your hands after touching surfaces/objects that may be contaminated can help prevent this type of transmission.
Q: What about infected pregnant women? Can they pass it on to their babies?
A. Yes. The virus can pass during or after birth through close contact.
Q: Can the disease be transmitted from animals?
A. Yes, it may. If someone comes into physical contact with an infected animal, such as some species of monkeys or a terrestrial rodent (such as the tree squirrel) transmission may occur.
Exposures can occur through bites or scratches, or during activities such as hunting, skinning, trapping, preparing meat or consumption of undercooked meat.
The risk can be reduced by avoiding unprotected contact with wild animals, especially those that are sick or dead (including their meat and blood). In Sri Lanka virus carriage among wild animals is not reported.
Q: Those with pets – are they also at risk? How?
A. The risk of pets getting infected is low unless the pet was in close contact with someone who had mpox. No pets were confirmed to have mpox during the global mpox outbreak in 2022.
Q: So how can we prevent getting infected or spreading the disease?
A. You need to avoid physical contact with infected persons until all lesions are completely healed. Persons with mpox need to self-isolate and cover skin lesions if they can. Healthcare workers attending to these patients must wear appropriate personal protective equipment as recommended. Regularly clean your hands with soap and water or an alcohol-based hand rub.
You should visit a doctor if you experience a rash particularly if you have had a recent foreign travel or were in close contact with someone who had so.
Most patients with mpox are managed with supportive measures. Antiviral treatment and vaccination are indicated in some circumstances..
Vaccination is used for individuals with high risk of exposure (including some healthcare workers) in some countries.
Q: Who can diagnose the virus? Any medical official or a virologist like yourself?
A. Medical doctors are capable of clinically suspecting mpox. This should be confirmed by laboratory tests.
Q: How is the diagnosis confirmed?
A. The laboratory confirmation of the diagnosis is essential and is a priority. All cases of suspected mpox should be tested for MPXV.
Facilities for testing are organised by the Department of Virology, Medical Research Institute. Colombo.
Testing of lesion material and throat swabs for the detection of viral genetic material by a method called polymerase chain reaction (PCR) is recommended.
Q: Are there other diseases that can have a similar clinical presentation?
A. Yes. There are many infectious and non-infectious causes for a blistering rash. One of the common differential diagnoses is chickenpox. Good clinical evaluation and laboratory testing are imperative to come to a diagnosis.
Q: What are the present gaps you see in our own health care system that prevents quality care being given to all persons infected by such infectious diseases?
A. Being a developing country, we face the challenge of maintaining the laboratory capacity to test a large number of samples, having the antivirals to treat complicated patients and having the hospital capacity to optimally isolate and manage these patients. However, health officials are making discussions with all stakeholders and are making strategic plans to face these challenges.
As you may remember, Sri Lanka had a good Covid-19 response with the scaling up of facilities in both laboratory testing and patient management facilities. This experience would be utilised should there be an emergency situation.
However, I must stress that mpox is not the new Covid–19 from what we know to date, as it is not spread as easily as Covid-19 between people.
Q: Your word of advice to all our readers out there on how to minimise risks of exposure to Mpox?
A. As of now, there are no documented cases on the island. However, there is a risk of importation of the disease from other countries.
Those who are visiting foreign countries, especially with African countries reporting the disease, need to be aware of the risks posed through prolonged close contact including sexual contact. Avoiding game meat is advisable.
It is very important that anyone who develops a rash and a fever seek medical attention particularly if they had returned from overseas or had been in close contact with someone who returned from overseas within the past 21 days.